A 21-year-old woman presented to the emergency department complaining of blurred vision and anisocoria that had started a few minutes after putting on her contact lenses.
On examination, she had isolated left pupil mydriasis that did not react to light or near stimulation and normal ocular motility.
Anisocoria is a difference in size between the pupils and may have many causes. The pupillary size is determined by the balance between the muscles dilator pupillae and sphincter pupillae, and the autonomic nervous system governs the action of these muscles. The parasympathetic nervous system contracts the pupil in response to light (light reflex) through the oculomotor nerve, and the sympathetic nervous system dilates the pupil.
There are many causes of anisocoria, and the approach consists of first determining which side is abnormal and then looking for other clinical features that might determine the diagnosis. If the anisocoria is more significant in the dark (when there should be pupil dilatation), the small pupil is the pathological one (miosis) and represents a predominance of parasympathetic nervous system activity (a lesion of the sympathetic or greater input of parasympathetic). If the anisocoria is greater in the light, the larger pupil is the pathological one (mydriasis), and this represents a predominance of sympathetic nervous system activity (lesion of parasympathetic pathways or greater input of sympathetic ones). If the anisocoria is equal in light and dark, and there are no other clinical features associated, this suggests a physiological anisocoria.
Mydriasis can be caused by ocular trauma or infections, Adie’s tonic pupil, third nerve palsies, or pharmacological agents. The history and examination reveal the cause in most cases. A history of ocular surgery or trauma should suggest traumatic mydriasis. The presence of a large pupil that develops a light-near dissociation and tonic response when going from light to dark after a few days suggests Adie’s pupil. The presence of diplopia, ptosis, and ophthalmoplegia suggests third nerve palsy. The absence of any ocular findings, and the presence of a fixed large pupil that goes back to normal after a few hours, together with a history of exposure to drugs that stimulate the sympathetic nervous system or block the parasympathetic nervous system, such as phenylephrine, scopolamine or atropine suggest a pharmacological cause for the mydriasis.
Since the patient had a normal eye examination, history of exposure to an anticholinergic drug, and the pupil returned to normal in a few hours, the diagnosis of pharmacological anisocoria was made.
Scopolamine (hyoscine) is an anticholinergic agent, usually prescribed to treat abdominal pain or prevent motion sickness. There are several reports of mydriasis after contact with a scopolamine patch, but none with storing pills in the same space as eyewear.
Pharmacological mydriasis is an important differential diagnosis of acute onset anisocoria, and a review of household medications use such as scopolamine is a crucial part of the evaluation [1].
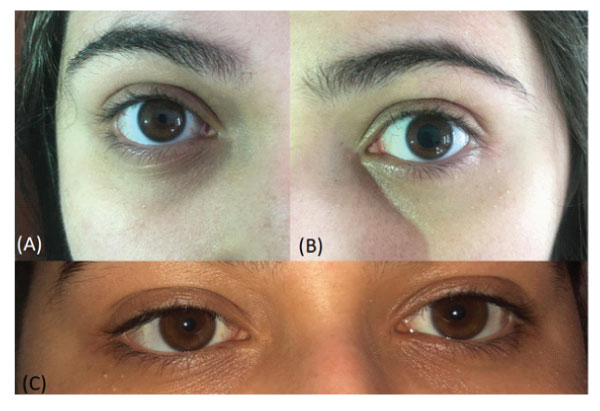
Figure 1: Anisocoria: Photos taken shortly before she went to the emergency (A- right eye and B left eye) and on the next day (C – both eyes). She had a largely dilated pupil that completely recovered.

Figure 2: Contact Lens Boxes: The contact lens box the patient showed after being asked if she had any contact to Scopolamine in her household. This was her father’s stocking of scopolamine pills.
Thaís Ecard Dacache – Reports no disclosures.
Victor Evangelista Rodrigues Pereira – Reports no disclosures.
Sofia Mermelstein - Reports no disclosures.
Patient Concent Form Available