Most cases of symptomatic hydrosalpinx requiring surgical treatment are caused by sexually transmitted diseases in adult population where the patient is sexually active. We wish to present a very unusual case of a left giant hydrosalpinx in a sexually inactive adolescent girl simulating an ovarian cyst pre-operatively and which was successfully treated with laparoscopy. A 15-yearold girl presented with left lower abdominal pain and mass. Patient had a past surgical history for a left lower laparotomy for primary pull through for Hirschsprung’s disease in infancy. Transabdominal ultrasonography revealed a multiloculated cystic lesion in the pelvis, and computed tomography imaging suggested multiloculated pelvic cyst. As the left ovary was not visualised separately; an initial impression of an ovarian cyst was made. Due to the ongoing abdominal pain and a palpable mass, laparoscopic surgery was performed. After aspiration and resection-marsupialisation of a cystic lesion, we confirmed that the left ovary was normal and that the cystic lesion involved the left fallopian tube, which had post-operative flimsy adhesions following previous laparotomy and pelvic surgery. Although relatively rare in postmenarchal sexually inactive adolescents, gynaecologists, radiologists and surgeons must still consider hydrosalpinx as a possible diagnosis when encountering an adolescent patient with lower abdominal symptoms, laparoscopy should be first choice and attempts should be made for preservation of adnexal structures.
Keywords: Adnexal Mass, Adolescent, Hydrosalpinx, Laparoscopy, Ovarian Cyst, Sexually Inactive
Isolated giant hydrosalpinx in postmenarchal sexually inactive adolescents is unusual, because the majority of hydrosalpinx cases are reported to be associated with sexually transmitted pelvic inflammatory diseases, in women during the most sexually active years. The results of surgical treatment of adnexal masses in young patients in a retrospective review of 48 patients treated between 2008 and 2015 showed great differences in ovarian preservation rate and laparoscopic procedure in patients treated by gynecologists and pediatric surgeons [1]. In the literature, there are reports of the midline pelvic cystic lesion at menarche in an adolescent female with hematometrocolpos and a case of hemorrhagic fimbrial cyst in a postmenarchal adolescent girl leading to fallopian tube torsion treated laparoscopically successfully but could find very few cases of the giant hydrosalpinx in an adolescent sexually inactive girl and hence wish to represent this interesting case treated laparoscopically and with ovarian and fallopian tube preservation to the best possible way increasing her fertility prospects later in the life [2,3].
A 15-year-old adolescent girl was admitted to our hospital with abdominal pain and a mass in the lower left quadrant, with no signs of peritonism or peritonitis. She was not sexually active and had no previous pelvic inflammatory disease (PID). Menarche took place at 13 years of age, her menstrual cycle was a painless regular 28-day cycle, and the last menstrual period had started before 15 days. She reported having no history of sexual intercourse. She had a past surgical history of primary pull through operation for Hirschsprung’s disease in infancy and arthroscopy of left knee and lateral release initially followed by medial patellofemoral ligament reconstruction due to recurrent dislocations.
Her vital functions were within normal range. Physical examination confirmed tenderness in the lower left quadrant of the abdomen, without a rebound tenderness. We noted the presence of surgical scars in her left lower abdominal quadrant with hockey stick smiling left Pfannenstiel incision and prominent scar. Her blood test showed hemoglobin 13 Gm/dl, White cell count 9.3x 109 /L, Platelets 262x109/L and urine laboratory tests normal including the inflammatory markers of C-reactive protein of 3 mg/l and the tumour markers of alpha-fetoprotein (AFP) was 12 ng/mL and b-Human Chorionic Gonadotrophin (B-HCG) was 6.0 mIU/m.
Abdominal ultrasonography revealed a complex intrapelvic cyst in the left adnexal region measuring 14 x 9 x 9 cm that was filled with clear fluid and intracystic septations, behind the normal bladder and in close proximity to the normal uterus, that mainly occupied left pelvis crossing the midline with the upper extent at the level of umbilicus. It had a hyperechoic/solid component deep in the pelvis. There was no demonstrable flow in this mass, and there was no ascites but the left renal pelvis was prominent without gross hydronephrosis. Left ovary could not be seen separately (Figure 1A and B). Our paediatric radiologists did not comment in their ultrasound reports presence or absence of normal ovarian tissue surrounding the ovary, namely, ovarian crescent sign (OCS) or a whirlpool sign of tubal torsion. The cystic lesion appeared to be benign and not associated with acute torsion and as the left ovary was not seen, left ovarian cyst was suspected.
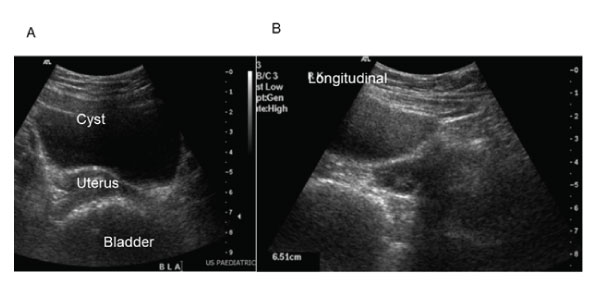
Figure 1A and 1B: Ultrasound scan of the pelvis showing bladder, uterus and cyst but no ovarian crescent sign or whirlpool sign.
The case was discussed at multidisciplinary oncology meeting in the presence of pediatric surgeon/urologists, adult urologists, gynecologists, oncologist, radiologists, pathologists and nurse practitioners and all agreed on cross sectional imaging in which pediatric team was in favour of magnetic resonance imaging (MRI) scan as the plan was to proceed with laparoscopy while rest were in favour of quick computed tom ography (CT) scan of the abdomen and pelvis as the waiting list for an MRI scan was longer and that she may not tolerate long periods in the noisy scanner. The abdomino-pelvic CT scan also identified a 14.3 x 11 x 7.8 cm multiloculated cystic mass arising from the pelvis from the left side of uterus without any internal calcification or fat (Fig. 2 A and B). There were enhancing septae but no clear enhancing solid component. The echogenic component on ultrasound may represent echogenic debris. The uterus was dextrorotated and appeared normal (Fig. 3). Left ovary was not identified and there was no free fluid or an ascites noted. Suture material noted at the ano rectal anastomosis of modified low Duhamel primary pull through for Hirschsprung’s disease in infancy. The neo-rectum was of normal calibre and contained faeces. The collapsed segment of sigmoid was closely related to the posterior wall of the cyst. Mildly prominent left pelvis noted, but no hydronephrosis. It was suspected that the mass might be a left benign ovarian cyst.
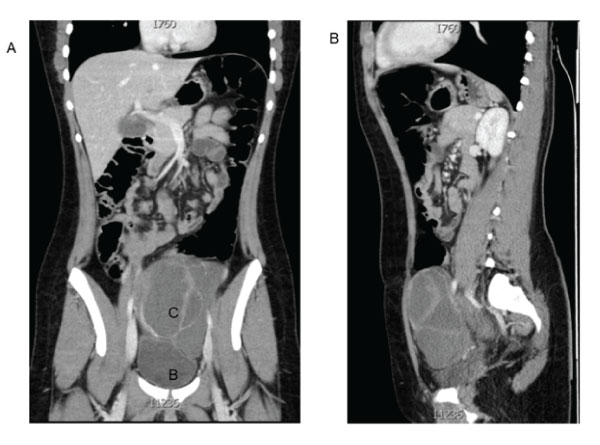
Figure 2A and 2B: Sagittal and coronal sections of abdomino-pelvic contrast enhanced CT scan showing multilobulated left pelvic cyst.
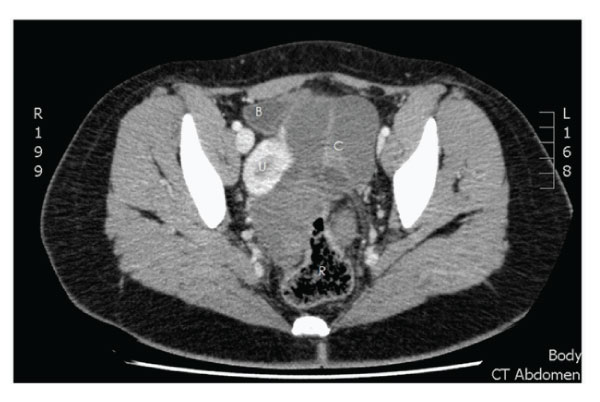
Figure 3: Transverse section of CT of pelvis showing the pelvic cystic © lesion on the left side displacing bladder (B), uterus (U) and rectum ®.
Pre-operative meeting was held with the patient and parents and indicated the uncertainty about the origin of the cyst which appeared benign and may be from left ovary or the adnexa and a decision of ovarian and/or adnexa preservation to the extent possible was the patient and parental preference to which we agreed. Although she had relative contraindication for laparoscopy due to previous pelvic surgery, our preference was initial laparoscopic approach and if any problems encountered then convert to open procedure. We strongly believe in ovarian preservation in benign cystic lesions as the tumour markers were normal and the CT scan has shown clear fluid.
Laparoscopic surgery was performed which revealed that the uterus and the right adnexa were normal in appearance. We could not confirm the left adnexa due to the post-operative adhesions and the multiseptated cysts occupying the left pelvic space. The cystic lesion was assumed to be a left ovarian cyst as left ovary cannot be seen initially even after the adhesion lysis. We aspirated off a clear fluid from one of the cysts and the emergency fluid cytology did not reveal any malignant cells and a frozen section was taken from the wall of the cyst which confirmed it to be fallopian tube structure.
The cyst was observed to have spread into the left broad ligament. As the cyst decompressed, we could ascertain the anatomy more clearly and could then see the left ovary and the fimbrial end of the tube was obscured in the post-operative adhesions. The cystic lesion appeared to arise from the central portion of the left fallopian tube and the portion of the tube closer to the isthmus appeared compressed but normal. We performed a left partial salpingectomy of the redundant giant cyst wall and confirmed that the tumor was part of the swollen left fallopian tube with a multilocular-type hydrosalpinx and the isthmic portion was well preserved. The left tubal fimbria of the hydrosalpinx could not be identified due to severe adhesion of the lesion to the pelvic peritoneum, indicating that occlusion at the fimbria of the left fallopian tube was the origin of hydrosalpinx. We did partial resection of very redundant giant cystic fallopian tube and salpingoneostomy with ovariopexy by suturing left ovary close to the normal appearing left fallopian tube near isthmus and intra operative methylene blue test showed tube patency.
The postoperative course of recovery was uneventful, and the patient was discharged on the 3rd day. At follow up ultrasound both ovaries could be seen with a follicular small physiological cyst on the right ovary. At 2 years following successful surgery she is asymptomatic, her periods are very regular, painless and moderate and she is pleased with overall good prognosis of this benign lesion and preservation of her fertility potential in the future. We discussed her case in the our audit meeting and decided to do trans anal modified Soave pull through procedure for Hirschsprung’s disease in future for a female patients in order to avoid such delayed complications of post-operative adhesions and gain hydrosalpinx.
Hydrosalpinx is defined as a distally blocked and dilated fallopian tube filled with serous or clear fluid. It has been reported in postmenarchal adolescent who are sexually inactive and had previous pelvic or inguinal retroperitoneal surgery causing fimbrial adhesions and blockade leading to hydrosalpinx [4]. It is generally seen after pelvic inflammatory disease (PID), commonly as a result of an ascending infection of Chlamydia trachomatis or Neisseria gonorrhoeae [5]. We have since last decade preferred primary transanal modified Soave pull through after a period of saline enemas to avoid any pelvic dissection and post-operative adhesions in female infants to avoid such late complications.
A hydrosalpinx usually remains a simple pathology and being very large size, a tubal torsion requiring surgery is quite rare in girls, and its pathogenesis in the our case seems to be secondary to prior pelvic surgery with subsequent post-operative adhesions leading to gradual blockade of the fimbrial end of the fallopian tube. The risk factors are generally very rare in adolescent girls; however, our patient had a history of pelvic major surgery in infancy, which is a known risk for both hydrosalpinx and tubal torsion [6].
The review of the surgical record of the patient suggested that her primary pull through operation for Hirschsprung’s disease was that of left lower laparotomy and Duhamel low pelvic anastomosis. The left tubal fimbria might have coalesced into the post-operative pelvic adhesions following the major pelvic surgical procedure in infancy, resulting in blockage of the left fallopian tube patency and eventually causing the hydrosalpinx.
Left sided lower abdominal and pelvic chronic pain in association with a palpable mass with normal inflammatory and tumor markers and no constipation related to previous Hirschsprung’s disease or any menstrual disorders, ovarian pathology seemed most common in the adolescent girl. Ovarian tumors are relatively easy to diagnose using transabdominal ultrasonography with a view of the intrapelvic unilateral lesion. However, as in the present case, it was difficult to accurately preoperatively differentiate a hydrosalpinx from an ovarian tumor or tubal torsion using transabdominal ultrasonography as there was no OCS or whirlpool sign of tubal torsion [7]. MRI is much more useful for making this distinction; however, MRI is not always performed in an emergency. Isolated tubal torsion with hydrosalpinx has been reported in the premenarchal girls [8]. Bertozzi et al. [9] reported just 20 cases in 26 years at five pediatric surgery units in a retrospective analysis. Recently, a case of tubal torsion associated with hydrosalpinx has been reported [10].
There are multilocular and unilocular types of hydrosalpinx. The salpingoneostomy in combination of left oopheropexy is a safe and effective surgical procedure used for correcting such lesions for the preservation of reproductive potential and avoids the need for salpingoplasty at a later date. Laparoscopic surgery, is our preferred and most desirable approach in such cases even if previous abdominal and pelvic surgery has been undertaken as our team is very experienced in pediatric laparoscopy which is less invasive, has less post-operative pain and the scar is minimal and was a preferred approach by our patient and parents as well. We believe that in ideal world the team leader should have pediatric surgical, pediatric urological gynecology, laparoscopy and adolescent transitional care experience in dealing with such lesions.
In conclusion, we believe that hydrosalpinx is a very unusual and rare lesion in the pediatric adolescent age group especially in the postmenarchal sexually inactive girls, and that it is almost impossible to accurately diagnose preoperatively, despite high index of suspicion due to giant size and quite often there is inability to see the ipsilateral ovary pushed aside deep in the pelvis. Gynaecologists, radiologists and surgeons should be aware about to the possibility of hydrosalpinx in adolescents having a history of primary pull through or other similar intrapelvic surgeries in the past even if not active sexually and consider it in the differential diagnosis of any cystic pelvic pathology in adolescent females. We strongly believe in laparoscopic intervention and ovarian preservation in such cases. With regards to retention of future reproductive capacity, pre-operatively, the patient and parents should be carefully informed of the possibility of needing at least a unilateral salpingectomy and the resulting risk of some loss of reproductive potential to avoid any communication gap and dissatisfaction or potential of any medico-legal actions later on.
Conflict of interest
The authors have no conflict of interest to declare. No funding source was involved in this study.
Ethical approval
All procedures performed on human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the parents of child prior to all the procedures. Parents were informed about the procedure.