A 32- year-old female presented to us with complaints of palpable masses over the neck region. The masses were painless and mobile in nature. There was no previous medical or surgical history. To evaluate the masses, she was advised ultrasonography (USG) of the neck. On USG, the right lobe of the thyroid appeared enlarged in size with an iso to hypoechoic lesion having areas of internal calcifications and increased internal vascularity [Figure 1A and B]. There were multiple oval to round hypoechoic lesions with internal cystic changes [Figure 1C] and vascularity noted in the right Ib, II and III levels. Fine needle aspiration cytology (FNAC) was done from the lesions to confirm the nature of the lesion. FNAC revealed smears of moderate cellularity showing clusters of follicular epithelial cells over a background of colloid mixed with blood [Figure 1D], categorizing the lesion into Bethesda-III [1], which has a malignancy rate of about 5-15%. The patient underwent computed tomography (CT) scan of the neck for further evaluation and to look for any extension or spread. On CT, a heterogeneously enhancing lesion was noted in the right lobe of the thyroid [Figure 2A and B]. Similar heterogeneously enhancing lymph nodes were present in bilateral level III [Figure 2C]. The patient was explained the clinical outcome and prognosis. She underwent a total thyroidectomy and neck dissection. The histopathology examination confirmed the diagnosis of concurrent papillary carcinoma (in normal thyroid & in the ectopic thyroid) with lymph node metastasis [Figure 2D]. She is kept on follow up and doing fine. Her serum TSH, T3, T4 levels, thyroid peroxidase and anti-thyroglobulin antibodies were within normal limits on follow up.
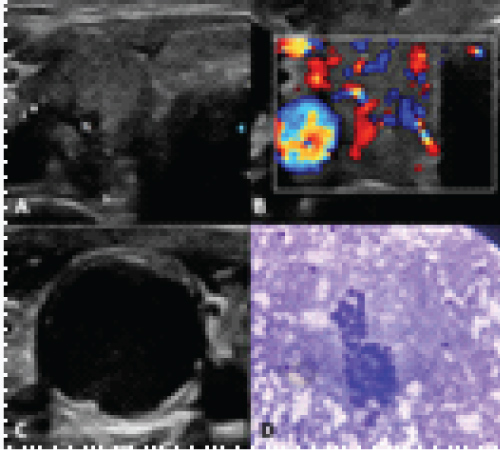
Figure 1:
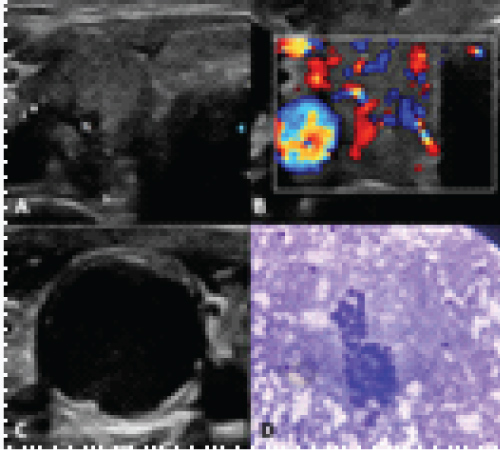
Figure 1A and B : A) Axial section from unenhanced CT neck showing bulky right thyroid gland (R) and heterodense lymph nodes (1 & 2). B) Axial section from the arterial phase of contrast-enhanced CT neck at the same level depicting the intense heterogeneous enhancement in the right lobe of thyroid (R) and 2 lymph nodes. C) Coronal section from contrast-enhanced CT of the neck in the venous phase showing multiple avidly enhancing lymph nodes. D) Biopsy image of a lymph node under 40X showing a papillary pattern of cells and nucleus showing clearing and grooving, signifying a papillary carcinoma thyroid.
The most common type of primary thyroid malignancy is papillary thyroid carcinoma (PTC). This form of carcinoma represents more than 70% to 90% of all thyroid malignancies [2]. PTC is a slowly progressive cancer and has a high survival rate [3,4]. Distant metastases have been observed in only 1% to 15% of patients diagnosed with PTC. Here we have discussed the case of a patient with concurrent PTC as well as lymph node metastasis. The PTC is usually transferred to the local lymph nodes via lymphatic drainage, and distant metastasis is extremely rare. Cervical lymph nodes are the most prone to metastasis, and 23% to 56% of patients with PTC have clinically significant lymph node metastasis which is a risk factor for high recurrence. In about 90% of cases of cervical lymph node prophylactic dissection, the histopathological results reveal lymph nodes metastasis. On ultrasound, when the lymph node undergoes cystic changes, it is said to be highly suggestive of papillary carcinoma thyroid. About 40% lymph nodes have a tendency to cavitate and undergo cystic degeneration [5].Other pattern of lymph node metastases are solid or partially cystic. The metastasis usually follows the same attenuation and post-contrast enhancement as the primary lesion. Hyper-enhancing lymph node metastasis may be observed in metastasis from papillary carcinoma thyroid, Castleman disease, lymphoma, Kikuchi disease and angioimmunoblastic lymphadenopathy. When FNAB is diagnostic for papillary carcinoma, total thyroidectomy is performed (because of its multifocal nature) with or without subsequent ablation with radioactive iodine [6].