Kikuchi-Fujimoto Disease (KFD) is an uncommon benign and self-limited condition characterized mainly by fever and lymphadenopathy. It rarely presents with life-threatening symptoms. Our paper reports the case of a 32 years-old woman who presented with acute laryngeal dyspnea and important neck-swelling, that later proved to be secondary to KFD.
Kikuchi-Fujimoto Disease (KFD), also known as Histiocytic Necrotizing Lymphadenitis, was first described in Japan in 1972, then has been reported worldwide. It is an uncommon, benign, and self-limited condition characterized mainly by fever, tender lymphadenopathy, and occasional rash. KFD is exceptionally revealed by a reactive laryngeal oedema, which was the case of our patient.
32 years-old Moroccan woman presented to the emergency room complaining of acute dyspnea for two days, dysphagia to liquids, and dysphonia, as well as a painful swelling on the left side of her neck that appeared 4 days earlier. On initial examination, the patient was conscious and well oriented, febrile, polypneic (25 breaths/min), with 97% oxygen saturation. Cervical exam showed a large lymphadenopathy at the left upper internal jugular nodes area. The mass was tender on palpation, rounded, firm, mobile, approximately 3cm in diameter, with inflammatory skin signs (pain, oedema, heat and redness). Oral cavity exam showed a slightly congestive and deviated left tonsil. Otoscopy and rhinoscopy were normal.
Flexible fibre optic Naso-pharyngoscopy revealed a gross oedema of the left hemilarynx that extended from the epiglottis to the left ventricular cord and left arytenoid cartilage. (Figure 1-a). Vocal cords were partially covered by the oedema. Nasopharynx and oropharynx were slightly edematous as well. Cervical CT scan found: a left pharyngo-laryngeal wall thickening, extended on 6 cm from cavum to glottis, with ipsilateral upper internal jugular lymphadenopathy with central necrosis and perilesional edema (Figure 2). Lab investigations showed hyperleukocytosis with 12000/mm3 and high C-reactive protein (CRP): 372 mg/L. Erythrocyte sedimentation rate (ESR) was raised at 49 mm/h. A fine-needle cytopuncture with histopathological examination revealed ganglionic lymphoid parenchyma with foci of eosinophilic necrosis surrounded by a palisade of lymphocytes, without epithelioid or giant cells, consistent with histiocytic necrotizing lymphadenitis of Kikuchi-Fujimoto (Figure 3).
The patient received intravenous corticosteroids (prednisolone 15 mg/kg per day for 5 days) and intravenous antibiotics (association of amoxicillin and clavulanic acid 3g per day for 7 days). Dyspnea and dysphonia disappeared within 24 hours of treatment. Flexible fibre optic Naso-pharyngoscopy at the third day showed complete resolution of edema (Figure 1-b). Lymphadenopathy decreased in size gradually and had fully disappeared at the 3 weeks follow-up. Regular surveillance for the past 11 months showed a complete recovery and no sign of recurrence.
Kikuchi–Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is a rare, under-recognized and selflimited syndrome that was first identified by two Japanese pathologists, Kikuchi and Fujimoto, in 1972 [1,2].
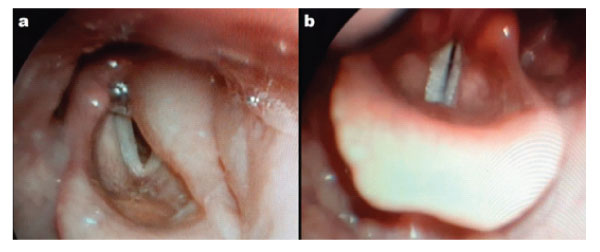
Figure 1: a) Flexible fibre optic Naso-pharyngoscopy on admission showing oedema of epiglottis and left arytenoid cartilage. b) Flexible fibre optic Naso-pharyngoscopy at day 3 of treatment, showing complete resolution of the pharyngo-laryngeal edema.
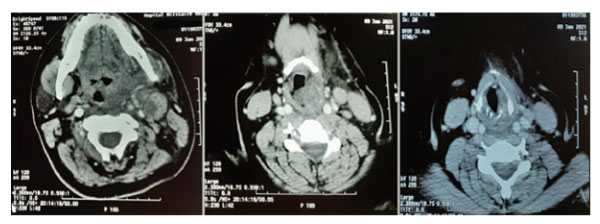
Figure 2: Tomodensitometry images showing a left lateralized pharyngo-laryngeal wall thickening, extended from cavum to glottis, with ipsilateral upper internal jugular lymphadenopathy with central necrosis and perilesional edema.
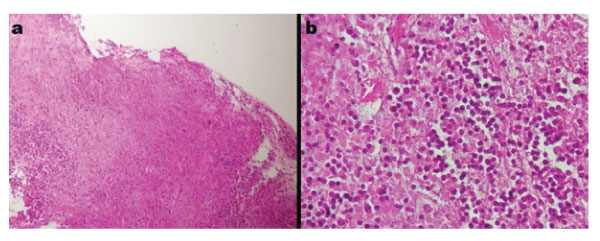
Figure 3: a) histologic image showing necrotizing lymphadenitis, magnification X10. b) histological image showing the polymorphic inflammatory infiltrate rich in neutrophils magnification X40.
The disease is mostly prevalent in Asiatic population, especially in Japan [3], but it has later been described worldwide. It was initially reported that KFD preferentially affects women (female/ male ratio: 4:1) [4]; however, recent studies, such as a 61 cases study in Taiwan [5], seem to indicate that the actual ratio is closer to 1:1 [4] . KFD most often affects adults younger than 40 years with a mean of 25.5 to 30.0 years [5].
The most common symptoms associated with KFD include lymphadenopathy, fever, erythematous rashes, fatigue, and arthralgia [6]. Laryngeal edema, dyspnea, or any acute lifethreatening symptoms such as our case are exceptional. To our knowledge, there has only been 3 similar case reports in literature [7,8,9].
There are no definite laboratory tests available for the diagnosis of KFD, but negative tests are important to exclude other disorders [5]. Diagnosis is based on histopathological examination of lymph node biopsy. It is characterized by lymphadenitis with paracortical coagulative necrosis, focal proliferation of histiocytes, and extensive karyorrhexis [3].
Differential diagnosis must be evoked, along the lines of malignant hemopathies, autoimmune diseases, and infections that could cause lymphadenopathy [8], particularly tuberculosis for our case, given that Morocco is an endemic country.
Treatment of Kikuchi disease is generally supportive. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to relieve the pain and fever. The use of corticosteroids, such as prednisone, has been recommended in severe extranodal or generalized Kikuchi disease [9].
However, some authors recommend expanding the indications for corticosteroid use to less severe disease [10]. In case of life-threatening symptoms, like acute dyspnea and upper airway obstruction, a broad-spectrum antibiotic and corticosteroid treatment can be started promptly [8], while waiting for histological results. Intravenous immunoglobulin (IVIG) can also be considered in case of recurrence or resistance to steroids [7].
Kikuchi disease is generally a self-limited disease with an excellent prognosis. Lymphadenopathy usually resolves within 1 to 6 months. However, about 3% of patients may experience recurrence [9].
Kikuchi-Fujimoto Disease is an uncommon, self-limited benign disease, but it can exceptionally manifest by life-threatening symptoms like acute laryngeal dyspnea. Diagnosis is based on histology findings. Although prognosis is usually good, some severe symptoms might require prompt management.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors report no conflict of interest.
Research Involving Human Participants and/or Animals
No human participants or animals were involved in this research.