Anorectal malformations (ARM) are rare occurrences characterized by the absence or abnormal localization of the anus and usually diagnosed and treated in the neonatal period. However, primary ARM causing secondary complications of secondary infertility can be observed in adult patients although we could not find any previously reported case. We wish to present a very unusual and interesting case of a neglected congenital ARM with recto-vestibular fistula (RVF) who developed secondary female infertility following fourth degree perineal tear at the first delivery followed by repeated and persistent genital tract infections to both partners resistant to several courses of antibiotics. Fertility clinic extensive investigations were all within normal limits and it was thought that the persistent genital tract infections secondary to complications of perineal tear and ARM with RVF were primarily responsible for it. The patient was referred to us for possible correction of the ARM with RVF preferably without a diversion colostomy. After a thorough colon and patient preparation, the patient underwent primary single stage anterior sagittal anorectoplasty (ASARP) without any covering colostomy and excellent cosmetic and functional results with the resolution of the secondary infertility in couple of months following definitive surgery. The second delivery could be done vaginally without the need for the caesarean section.
Keywords: Anorectal Malformation (ARM); Anterior Sagittal Anorectoplasty (ASARP); Female Infertility; Genital Tract Infections; Pelvic Inflammatory Disease; Recto-Vestibular Fistula; Secondary Infertility
Fertility is the capacity to establish a clinical pregnancy. Infertility can be primary or secondary. Primary infertility is when a pregnancy has never been achieved by a person, and secondary infertility is when at least one prior pregnancy has been achieved. Primary infertility is a disease characterized by the failure to establish a clinical pregnancy after 12 months of regular and unprotected sexual intercourse. Secondary infertility happens when a patient can't get pregnant or carry a baby to term after the patient have been pregnant before and had a baby when the couple have been unsuccessfully trying to conceive for six months to a year of regular and unprotected sexual intercourse. It is estimated to affect between 8 and 12% of reproductive-aged couples worldwide [1]. Secondary infertility is the most common form of female infertility around the globe, often due to disease related and reproductive tract infections [2,3]. Worldwide >186 million people suffer from infertility, the majority being residents of developing countries. The three major factors influencing the spontaneous probability of conception are the time of unwanted non-conception, the age of the female partner and the diseaserelated infertility. We present a very unusual and interesting case of neglected congenital ARM with RVF in an adult female who suffered fourth degree perineal tear at first delivery leading to flooding of genital tract of both partners with recurrent genital tract infections and secondary infertility which was resolved by performing single stage ASARP in supine lithotomy position without any covering diversion colostomy with excellent cosmetic and functional results and resolution of the secondary infertility.
1.Case Report
A G1P1A0L1 status 31-year-old female patient and a mother of a 4-year-old girl and her partner presented with recurrent and persistent genital tract infections despite several courses of antibiotics and antifungals including topical imidazole and hydrocortisone and oral fluconazole, metronidazole, co-amoxiclav, cephalosporins, ofloxacin, doxycycline and azithromycin and secondary infertility since she had baby girl delivered vaginally 4 years ago which was complicated by fourth degree perineal tear which made the existing ARM with RVF worse with constant constipation, gas, and defecation through the vagina. At birth she was diagnosed with ARM with RVF and was referred to senior professor and head and a general surgeon with pediatric surgical interests and they have done dilatation and cut back procedure which was in routine practice in general surgery in those days. The patient, who did not seek medical assistance thereafter for various reasons (personal, family, social, education and availability of experts who can reconstruct these problems without a diverting colostomy) until the first delivery at which congenital ARM with RVF and the intrapartum complication of fourth degree perineal tear were evident. Patient was advised surgery to correct them but all surgical consultations so far have opted for three stage surgery but patient did not want colostomy.
Husband had florid candida balanitis resistant to most antifungal and antibiotic treatments including topical imidazole and hydrocortisone and oral fluconazole, metronidazole, flucloxacillin and clarithromycin. The physical and abdominal examination of the patient was normal. The perineal examination revealed an ARM with a RVF, and fourth degree perineal tear through the mucosa of the fistula and ended in the distal vagina (Fig.1 A).
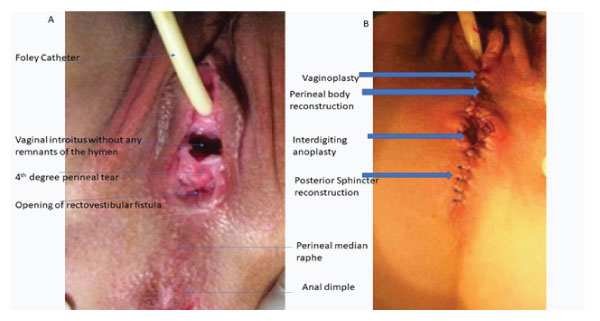
Figure 1A: Perineal anatomy before surgery.
Figure 1B: Perineal anatomy after surgery.
Both partners have extensive laboratory investigations related to secondary infertility which were all within normal limits. Abdominal ultrasonography (USG) was normal. Plain abdominal radiograph showed rectosigmoid loading with reversal of rectosigmoid ratio. Barium enema showed huge dilatation and rectosigmoid loading and there was ileocecal reflux into the terminal ileum. She was therefore given laxatives and micronutrient therapy orally and daily warm saline enema through the rectovestibular fistula to clean the bowel and reduce the rectosigmoid dilatation.
Following pre-operative patient and colon preparation, patient underwent on table preoperative bowel irrigation with normal saline, examination under anesthesia including measurement of the length of the rectovestibular fistula, perineal sphincter muscle complex stimulation to accurately locate the position of the external anal sphincter and vaginoscopy in lithotomy position A small pillow was placed under the buttocks so as to enable clear visualization of surgical field in the perineal area. The legs were supported by soft cotton rolls to prevent injury to the hip joint and nerve damage.
Separation of the anterior wall of the rectum from the posterior wall of the vagina was the most crucial and important stage of procedure. Stay sutures at 3 to 4 mm intervals were placed at the mucocutaneous junction of the RVF. Then, a vertical incision was made through the layers posteriorly from the RVF through the perineal median raphe to just beyond the anal dimple. The incision was deepened, and all tissues were divided strictly in the midline, and the anterior wall of the rectum was exposed. The external sphincter muscle complex was prepared and an equal amount of muscle were left on both sides. Posterior to rectum, there is a well-defined plane, and with sharp and blunt dissection, starting posteriorly followed by lateral aspect, the posterolateral rectal wall was separated from the adjacent musculature. Gentle finger dissection with restricted use of cautery was done for inflicting minimal damage to neurovascular bundles/fibers. The rectum was separated from the vagina up to the peritoneal reflexion. It requires extreme patience, gentle and sustained traction on the stay sutures and proper assistance and experience. Mobilization of the rectum was performed circumferentially till the fistulous opening reaches the proposed site of neoanus without tension.
The posterior wall of the distal vagina, vestibule and the vaginal introitus were reconstructed with fine sutures, followed by repair of perineal skin. After the rectum was fully released, the perineal body was reconstructed. The rectum was placed in the center of the muscle complex. Anterior aspect of the muscle complex was then approximated taking bowel wall (seromuscular) in the stitches, craniocaudally by interrupted suitably sized absorbable sutures. The midline of the skin was closed, and the cruciate interdigiting mucocutaneous anorectoplasty was completed by suturing the rectal section to be anatomized to the skin so that it remained within the borders of the external sphincter (Fig. 1B). Histological examination of the resected rectovestibular fistula showed only few ganglion cells even at the upper level of resection lines and was concluded associated hypoganglionosis as congenital colorectal motility disorder.
During the postoperative period, the patient was allowed to take plenty of liquids only orally for five days. Because no complications developed, the patient was discharged on the 6th post-operative day. With the interdigiting mucocutaneous anorectoplasty we do not do any regular post-operative anal dilatations. Follow up visit was scheduled at 3 months but the patient with family visited at two months with pleasant surprise and sweets that the patient was able to conceive and this time it was baby boy. The pregnancy was monitored, was uneventful and the baby boy was delivered by spontaneous vaginal delivery with a planned episiotomy. Follow up at last visit after 25 years of surgery, the patient defecates regularly once a day and maintains anal continence of gas, liquids and solids without any anal stenosis or prolapse of the mucosa and perfect healing of perineal wounds (Fig. 2). Their son has graduated from medical college and currently doing internship.
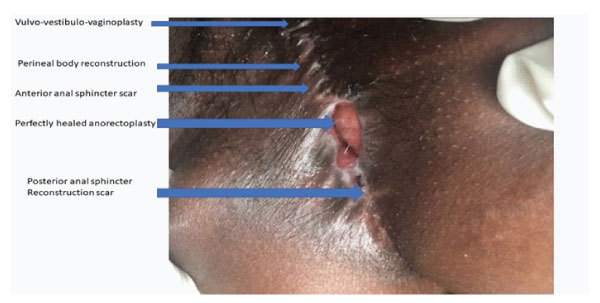
Figure 2: Post-operative long term follow up photograph. Note no excoriation in perianal region and perfect healing of the perineal scar.
Secondary infertility in developing countries is mostly attributable to blockage of the fallopian tubes due to adhesions caused by reproductive tract infections [4]. It is feasible to gauge national levels of primary and secondary infertility from population-based surveys including a birth history. The prevalence of infertility of pathological origin is so high in subSaharan Africa that infertility is not merely an individual concern, it is a public health problem [5]. The experience of infertility is a stressful condition itself. This becomes particularly traumatic with previous pregnancies ending up in abortions, stillbirths and neonatal/infant deaths. However, it subjects the woman to contempt and exploitation resulting in severe psychological stress [6].
Clinical manifestations can vary from mild forms that require only minor surgery to more complicated cases that must be managed with multi-staged surgery. A patient with an anorectal anomaly seeking medical assistance and treatment for the first time in adulthood is a rare occurrence and we could not find any similar cases presenting with fourth degree perineal tear and secondary infertility. ARM include a number of congenital defects and various types of urinary and/or sexual malformations [7]. The recto-vestibular fistula in our patient is the most commonly observed anorectal defect in female pediatric patients with anorectal malformations while the presentation and complications of fourth degree perineal tear and secondary infertility are the rarest of the lesions.
In order to select the best treatment option in adults with ARM with RVF and to achieve a satisfactory result; the type and size of the defect should be carefully evaluated, and the anatomic structure and borders of the perineum and pelvis should be examined in detail. In these patients, concomitant anomalies should be considered and the necessary tests should be performed. The management of such complex lesions needs attention of the multidisciplinary expertise and the other departments, including mainly pediatric surgery, gynecology, and urology, should be involved in the systemic evaluation of adult patients with ARM [7].
Basic objectives in female ARM with RVF correction are to facilitate adequate separation of the vagina from the rectum, adequate downward mobilization of rectum, vulvo-vestibulovaginoplasty after separating them from RVF, reconstruction of perineal body, proper separation and identification of sphincter muscle complex, passing rectal tube through sphincter muscle complex and perform a tension-free anastomoses of rectum with skin-the anorectoplasty.
The management of this form of ARM has undergone several changes. Surgical techniques used for the treatment of rectovestibular fistula and low-type anomalies in females include anal dilatations, cutback procedure, perineal anal transposition, neutral sagittal anorectoplasty, Y-V plasty, minimal PSARP, sacroperineal repair, and ASARP. Once the posterior sagittal anorectoplasty (PSARP) for all ARM came into practice in 1980s. it has been gold standard. Currently, there are three different approaches to resolve this ARM, namely ASARP, PSARP and laparoscopic-assisted anorectoplasty (LAARP). We prefer the ASARP as it combines the best of all worlds and the comfortable supine lithotomy position is anesthetiic friendly and avoids complications associated with prone jack-knife position, incision is small with minimum invasion, adequate exposure, normal anatomical orientation and technically easier with no division of levator ani muscle, with minimal dissection of the external sphincter and easier dissection, separation and reconstruction of the vagina, vestibule, vulva and rectum, precise positioning of rectum in the sphincter muscle complex and accurate reconstruction of perineal body, comfortable position of operating surgeon ergonomically and less chances of wound infection [8]. ASARP technically precise but difficult and requires years of experience to master the surgery and requires preoperative bowel preparation and postoperative bowel management for avoiding any bowel movement for 5 days [9].
Postsurgical prognosis is better in adult patients in whom the gluteal cleft is fully developed beside the sacrum and the normal gluteal muscle mass, the nerves are intact to maintain the anal reflex, and the voluntary perineal muscles are visibly contractile. A colostomy may not be necessary in adult patients with optimal passages or in whom the passage is maintained at the desired level through medical methods and single stage reconstruction may be feasible [10]. ASARP is an excellent procedure for RVF as it provides optimal correction with minimal sphincteric damage, without additional complexity or difficulties. Primary ASARP is a quick and effective technique and doesn’t require colostomy if performed after due preoperative patient and gut preparation and performed by an experienced pediatric surgeon.
We recommend health education to professions, public and parents for early diagnosis during neonatal examination and appropriate treatment as the management of this anomaly has undergone change with an emphasis of early and aggressive surgical correction to avoid long term morbidity. ASARP is a safe and very effective technique with optimal cosmetic, functional and patient/parent satisfaction outcome, even in late detected and complicated one like our case, can be treated effectively in one stage without preliminary colostomy. We prefer ASARP over PSARP approach as the incision is smaller, with minimal dissection of the external sphincter and easier dissection, separation and reconstruction of the vagina and rectum. Our case is a usual reminder that primary ASARP is useful for congenital ARM with RVF as well as for the acquired post obstetrical perineal body defects such as RVF and chronic third and fourth-degree lacerations that are most often secondary to vaginal delivery, gynecologic surgery, and inflammatory bowel disease. Key concepts include a tensionfree repair of the vulvo-vestibulo-vaginoplasty, perineal body reconstruction, placement of the neorectum and anus in the centre of the sphincter muscle complex, a meticulous hemostasis, and perioperative bowel management.
We care grateful to the son of our patient for searching the literature and bringing its rarity and practical utility of this primary single stage procedure and motivating us to report it.
Conflict of interest
The authors have no conflict of interest to declare. No funding source was involved in this study.
Ethical approval
All procedures performed on human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the parents and all the relatives involved prior to all the procedures. Parents and all involved parties were informed about the procedure.