Hemophilia B, also known as Christmas disease, is an X-linked disorder caused by either the absence or reduced biosynthesis of clotting factor IX. This disorder affects approximately 1 in 30,000 male individuals world- wide. It is five times less common than hemophilia A.
Hereby we report a case of Haemophilia B in a 3-month-old infant with unusual presentation, in whom a diagnosis was made based on coagulation profile and later confirmed by Factor 9 level.
Therefore, we emphasize the importance of early recognition and diagnosis of haemophilia despite the rare presentation. Furthermore, early recognition of haemophilia would lead to safe and effective treatment and better outcome.
Keywords: Haemophilia B; Bleeding; Diagnosis; Children; Factor 9.
Hemophilia is a rare X-linked congenital bleeding disorder characterized by a deficiency of coagulation factor VIII (FVIII), called hemophilia A, or factor IX (FIX), called hemophilia B.
Hemophilia A is much more common than hemophilia B. Hemophilia A is estimated to account for 80%-85% of all hemophilia cases; hemophilia B is estimated to account for 15%-20% of all hemophilia cases [1]. It can be categorized according to severity into severe, moderate, and mild based on the factor plasma levels of 1% or less, 2 to 5% and 6 to 40%, respectively [2]. The presentation varies according to the severity of the disease. The prevalent symptom is spontaneous or post-traumatic hemorrhage, musculoskeletal bleeding being the most common[3]. We are reporting a case of hemophilia B in a 3-month-old male infant with unusual presentation, with multiple body sites mass swellings, found to show atypical features of hemangiomas, initially diagnosed, and treated as a case of cellulitis. Our aim is to highlight the different presentations of hemophilia for early diagnosis.
A previously healthy 3 months old Sudanese male infant, born as a product of non-consanguineous marriage, presented to our hospital with multiple areas of swelling in the body. 2 weeks prior to admission, the child initially had a swelling in the left cheek (figure1), it was around 3x2cm, mobile, non-painful, not tender with no overlying erythema. He was seen in a private clinic, Found to be febrile, an ultrasound was done and showed an avascular complex cystic mass. The patient then received antibiotic (azithromycin) treatment for 1 week as outpatient as the private clinic physician considered the possibility of these lesions to be infective in nature, however the patient condition did not show any improvement as the patient developed another lesion on the dorsum of the right hand (figure2) and sought medical advice in Tawam hospital, the new lesion was measuring around 3x3x2 cm rigid, tense mass associated with erythema and redness, with restriction in fingers movement, but no warmth or tenderness.” On the day of admission, the child developed one new swelling, on the left upper side of the chest (figure3), small around 1x1 cm, mobile, non-tender mass with overlying bluish discoloration.

Figure 2: Right hand swelling: 3x3x2 cm rigid, tense mass associated with erythema and redness, with restriction in fingers movement, but no warmth or tenderness.

Figure 3: Left upper chest swelling: small around 1x1 cm, mobile, non-tender mass with overlying bluish discoloration.
The child has been otherwise healthy, active with no other complaints, thriving well and meeting his developmental milestones. The remaining of his past histories and physical examination, were unremarkable. He had no history of bleeding tendency and no family history of any bleeding disorder, and the patient has no siblings.
Initial laboratory workup including Compete Blood Count (CBC), C-reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR) were reassuring and not suggestive of an inflammatory element.
Ultrasound imagining of the lesions (figure 4), showed evidence of well defined, capsulated, localized complex soft tissues mass lesion, with internal echogenic content showing some internal vascularity. The US picture was highly suggestive for vascular lesions, including infantile hemangioma. A Magnetic Resonance Imaging (MRI) of the brain, chest, abdomen, and upper limbs (figure5) was done and showed no internal hemangiomas, only three subcutaneous soft tissue lesions in the areas mentioned before, with varying age hemorrhagic components, presence of hemosiderin in the lesions indicating bleeding, highly suggestive of multiple hemangiomas.
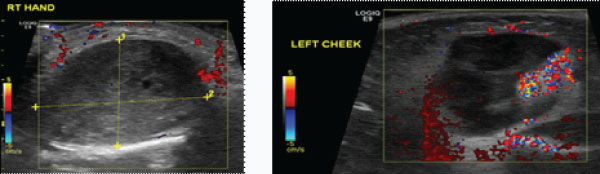
Figure 4: Ultrasound imagining of the lesions, showing evidence of well defined, capsulated localized complex soft tissues mass lesion with internal echogenic content showing some internal vascularity seen in the left side of the cheek, dorsum aspect of right hand and supra clavicular area measuring 17x16x15 mm, 3x3x2 cm and 1x0.5x0.5 mm respectively.

Figure 5: Magnetic Resonance Imaging (MRI) of the brain, chest, abdomen, and upper limbs, showing well-defined lobulated focal lesion, in the left cheek measuring about 23 x 19 mm with 2 component of different signal intensities. The medial component showing hyperintense signal in T1, T2 and FLAIR which suggestive of haemorrhagic elements while on the lateral part of the lesion it appear hypointense. The second lesion seen in the dorsum of the right hand, it is a well-defined measuring 26 x 28 mm, and other smaller lesion noted in the left supraclavicular area all suggestive of multiple haemangioma with varying age haemorrhagic components. No internal haemangioma seens.
Coagulation screen (table 1) was sent for the infant in view of the hemorrhagic component seen in the imaging and showed to have an elevated APTT of 121.3 seconds, with normal PT and INR. Repeated APPT confirmed prolongation of 103.5 seconds with 100% correction in mixing study. Factor VIII level and IX level were then ordered and factor IX came to be 0.5%, confirming the diagnosis of severe Hemophilia B. No other hematologic disorders were investigated such as von willibrand disease.
Table 1: Showing the results and interpretation of the patient’s coagulation profile, compared with the age specific normal values.
Coagulation profile |
1 month – 1 year (Age specific coagulation values) |
||
PT |
11.8 sec |
Normal |
13.1 (11.5–15.3) |
INR |
1.12 |
Normal |
1.00 (0.86–1.22) |
APPT |
103.5 sec |
High |
39.3 (35.1–46.3) |
APPT Mix |
26.7 sec |
Normal |
- |
Fibrinogen level |
3.45 g/L |
Normal |
2.42 (0.82–3.83) |
D-Dimer |
2.570 mg/L |
High |
0.22 (0.11–0.42) |
Factor IX level |
0.50% |
Severely low |
0.71 (0.43–1.21) (U/mL) |
Factor VIII level |
162.50% |
0.94 (0.54–1.45) (U/mL) |
Regarding the other possible differential diagnosis for the patient, we entertained the possibility of Cellulitis of the right hand as the patient was having swelling, erythema, and some hotness, therefore, the child was started on clindamycin initially but there was no change noted in the lesion. The possibility of Abscess and osteomyelitis were also unlikely based on the clinical picture, physical examination, and MRI findings.
After diagnosing the infant with Hemophilia B, he remained clinically stable with no active bleed; therefore, no Factor IX replacement was needed per the multidisciplinary team agreement, also no prophylaxis was started to avoid medication related side effect including anaphylaxis on early development of inhibitor. Parents were instructed to seek medical attention immediately in case of any trauma or new active bleed.
Outpatient clinic follow-up was continued in the hematology clinic of Tawam Hospital at 1 week, 2 months, 3 months, and 4 months post hospital discharge. The left cheek and upper chest swellings were resolved completely by the 2 months visit, while the considerably larger right-hand swelling showed complete resolution by the 3 months post-discharge clinic visit.
The patient had an ER visit two months following the initial presentation due to gum bleed after accidently hitting his head with the edge of the bed and he received one dose of IV Tranexamic Acid after which the bleeding stopped; therefore, the patient was discharged home. Approximately 12 hours later the patient was brought back again to ER due to recurrence of bleeding, for which he received Factor IX complex along with Tranexamic Acid IV and was discharged when the bleeding stopped. Two days later the patient presented a third time with bleeding from the same site of the formed clot. At that time, he was noted to have hemoglobin drop from 104 g/L in the initial ER visit to 82 g/L, therefore the child was admitted to the hospital where he received a second dose of Factor IX complex and Tranexamic acid. The patient was discharged after 2 days when the bleeding has completely resolved.
Early identification of the disease can prevent complications, therefore being familiar with different disease presentations will help in early diagnosis and hence better outcome.
Diagnosis of hemophilia is based on medical history, clinical examination, and laboratory investigations. Medical history should include history of bleeding after previous surgery or trauma, drug history, family history of bleeding abnormalities and symptoms associated with potential bleeding disorders. Diagnostic laboratory investigations in hemophilia B can be a prolonged activated partial thromboplastin time (aPTT), normal bleeding time (BT), normal prothrombin time (PT) and low factor IX [4].
The typical presentation varies according to the degree of the severity. In mild hemophilia, bleeding will present only after significant trauma or surgery, spontaneous bleeding is uncommon, and typically the diagnosis is made incidentally. In moderate hemophilia, bleeding usually presents after trauma, injury, dental work, or surgery. Recurrent joint bleeding may be present in up to 25% of cases, and the diagnosis usually gets delayed until late childhood or adulthood. While in severe hemophilia, bleeding will present spontaneously and will appear early in life due to a lack of transmission of coagulation factors trans-placentally [5].
We have reviewed case reports of hemophilia with rare or unusual presentations. Ibrahim Aliyu and Zainab F Ibrahim [6] reported a case of a 7-month-old male infant with massive spontaneous truncal intradermal bleeding presenting with jaundice and loss of consciousness. The diagnosis was made based on prolongation of the activated partial thromboplastin time (APTT) and the response to factor VIII concentrate replacement therapy, as factors VIII or IX assay could not be done due to nonavailability of the test.
The unusual presentations of hemophilia can be life threating. Sook-Hyun Park, M.D., and Byung-Ho Choe, M.D [7]. reported a case of a male infant who developed repetitive hematemesis on the first day of life. His initial level of coagulation factor IX was 1.9%, and he was diagnosed with moderate hemophilia B. Similarly, Lisa M. Pace, Andrew Y. Lee, Sfurti Nath, Neil B. Alviedo [8] reported a life threating presentation of hemophilia B in a premature, monochorionic-diamniotic twin born at 29+3 weeks gestation with acute life-threatening pulmonary hemorrhage with no family history of bleeding disorders, after he developed apneic episodes along with tachycardia in day 7 of life. Another unusual presentation of hemophilia B is a rare case reported by Saurav Mittal, MS (Ortho), Sumit Arora, MS (Ortho), DNB (Ortho), Shilpa Khanna, MD (Peds), Lalit Maini, MS (Ortho), and V. K. Gautam, MS (Ortho), DNB (Ortho), MNAMS [9] of a 10-year-old boy with a 6-month history of swelling and pain around the left knee joint and proximal leg presenting directly as a case of pseudotumor without any previous history of bleeding disorder who was found to have factor IX assay of only 1.1% activity.
In our patient the classical presentation of hemophilia was not present as well as negative family history, but the imaging findings of hemangioma guided us to look for underlying bleeding disorder. There were no similar presentations in previous case reports. Therefore, unusual, or spontaneous bleeding in pediatric age groups should warrant us to investigate for coagulation factor deficiency, regardless of the family history. This can result in prompt diagnosis and treatment.
Hemophilia B, also known as Christmas disease, is a rare X-linked congenital bleeding disorder. It is characterized by varying degrees of severity which correlates with the presenting symptoms. Due to the low incidence of Hemophilia, which makes it a rarely- suspected diagnostic possibility, leading, ot infrequently, to a diagnostic delay. We report a case of Haemophilia B in a 3-month-old infant with unusual presentation to emphasize the importance of early recognition and diagnosis of haemophilia despite the rare presentation as this would lead to safe and effective treatment and better outcome.
Funding:Nil