- Review Article
- Mary Anbarasi Johnson1,*
- 1 Professor and Head Pediatric Nursing Department CMC Vellore, Dr. MGR Medical University/ College of Nursing CMC Vellore, Tamil Nadu, India.
- *Corresponding author: Mary Anbarasi Johnson, Professor and Head Pediatric Nursing Department CMC Vellore, Dr. MGR Medical University/College of Nursing CMC Vellore, Tamil Nadu, India, Email: mary1967cmch@yahoo.com; Mary.anbarasi@cmcvellore.ac.in.
- Received: 25-07-2022; Accepted: 01-08-2022; Published: 04-08-2022.
Abstract
Pain is subjective and is usually expressed by the caretakers in younger children. Pain response is unique for each child. Different pain assessment tools need to be used for different age group of children. Nurses need to be very sensitive in the assessment and management of pain. Nurses need to know and explain about pain they need to be able to discuss about the various tools used in the assessment of pain in different age group of children. They also need to be able to enumerate the signs and symptoms of pain in children.
Keywords: Opioids; Pethidine; Pain Ladder; FLACC Scale
Introduction
Pain is not just a sensation but also an emotion, which has long been under recognized and untreated in the pediatric population. In the past, it was assumed that neonates and young infants were unable to recognize pain as their nervous system was not fully developed; and hence did not suffer. However, with the advancement of scientific knowledge, we know today that even premature babies have the capacity to feel and respond to pain. Infants and young children also tend to have a more robust inflammatory response and coupled with the lack of central inhibitory influence, they are likely to experience more pain than adults do. Pain experiences, including acute and chronic, are common in infants, children, and adolescents [1-7]. Data from children’s hospitals reveal that pain in pediatric patients is common, under–recognized and under–treated [8-17].
In view of this, pediatric pain needs to be assessed and managed appropriately. However, pain management in the pediatric population has long been recognized to be inadequate. The main reason is because pediatric patients often lack the ability to communicate the source and severity of their pain. Therefore, children are often given minimal or no analgesia for procedures that would routinely be treated aggressively in adults. In addition, one is also often faced with multiple challenges when managing pain in children due to the wide range of physiological, pharmacological, cognitive and developmental differences between the various age groups. Health care professionals need to be aware of these differences and the limitations in any method used.
These challenges should not however dissuade us from measuring pain in the pediatric population because evidence has shown that untreated pain has a negative impact on the child. For example, painful experiences in early life can lead to lowering of pain thresholds for months after a procedure. Unrecognized acute pain can become established, severe and difficult to control. Unrelieved pain can have negative physical and psychological consequences, which may lead to extended lengths of hospital stay with resultant service and cost implications.
Therefore, we hope that as pain becomes recognized as the 5th vital sign, pain recognition and management in the pediatric age group will progressively improve. Health care professionals who care for children should become more sensitive and aware of the possible existence of pain in this age group (even when the patients are unable to verbalize pain) and take efforts to institute more effective procedures and processes to minimize pain, and offer a more holistic medical management.
Approach to Assessing Pain in Children
We need to be able to perform ongoing assessment of the presence and severity of pain, as well as the child's response to any treatment instituted if we wanted to treat pain effectively. There are various ways to approach a child in pain and this is a suggested approach using the acronym 'QUESTT'.
QUESTT: Question the child Use pain-rating scales Evaluate behavioral and physiological changes secure the parents' involvement Take the cause of pain into account Take action and evaluate results
Question the child
- Every child is different and the first step in assessing pain in children is to take a pain history. Discussions should be made directly with the child when possible but in cases where a child is not able or unwilling; an attempt should be made to obtain the caregiver’s opinion.
- It is important to remember that the way in which a child expresses pain is not only affected by their chronological age or cognitive development; but also by individual differences and cultural factors.
- Also remember that children need opportunities and time to talk about their pain. This might be difficult in a busy ward and some children might not like to disturb staff and hence children should be encouraged.
- Health care professionals are advised to listen and believe a child’s description of pain as it has been shown that children can accurately identify the location and severity of pain when they are encouraged to do so.
- Doctors can take a pain history by asking “Does anything hurt” and then using the following acronym PAIN: 0 P : Place or site of pain “Where does it hurt?” 0 A : Aggravating factors “What makes the pain worse?” 0 I : Intensity “How bad is the pain?” 0 N : Nature and neutralizing factors “What does it feel like” (a body chart might help children describe their pain) “What makes the pain better?”
- Some children may have difficulty communicating and this group needs particular attention. Examples of this group are preverbal children, children on ventilators or those who are cognitively impaired, psychotic or severely emotionally disturbed children, those who do not speak the same language or have significantly different family/cultural background from those of the health care provider.
Use pain rating scales
- Children have been shown to be able to reliably report their pain using ‘Self report tools’ from as young as the age of 4 years.
- However, the tool/rating scale that is used must be individualized and appropriate for the child’s developmental level, personality and condition.
- It is important to remember that these tools should never be interpreted singly but used in conjunction with the child’s self–report, with parents’ assessment as well as health professionals’ assessment of a child’s pain.
Evaluate behavioral and physiological changes
- Changes in behavioral and physiological measures have been shown to be important proxy measures for pain especially in younger children, infants and neonates who are either unable to or refuse to communicate with health care professionals.
- Behavioral measures include assessment of facial expression, crying, and body posture, response to questions, activity and appearance. Changes in behavior may indicate changes in pain intensity. Beware that some children might not exhibit pain by crying but rather by being unduly quiet or being restless.
- Physiological changes are also thought to be associated with pain and therefore suggested as indicators of pain. Examples of physiological measures include heart rate, respiratory rate, blood pressure and presence of palmar sweating and oxygen saturation. However note that these physiological changes should not be used as an isolated assessment of children’s pain but rather as part of a more comprehensive approach.
Secure the parents’ involvement
- Parents should be involved in pain management of their child.
- Parents can often accurately judge their children’s pain and thus their involvement can lead to early recognition and more accurate assessment. However, parents’ assessment should not override the child’s self–report.
- Although it is true that children may verbalize or display more distress in the presence of their parents, there is evidence (Craft 1990) that children find their parents’ presence , particularly the main carer a helpful contribution to pain management.
- Similarly, one study has shown that if parents are kept well informed and assist in the management, children suffer less pain.
Take the cause of pain into account
- It is important to search for any possible simple reversible causes of pain before starting any treatment for e.g. a tissue iv line whereby simple removal may alleviate the pain. Another example is a post op child with abdominal pain might not actually be having pain from the wound but rather discomfort from a distended bladder due to urinary retention.
- Also consider if anxiety is the source of the complaint e.g. anxiety being in a new environment or separation anxiety when parents leave the child in the hospital whilst they go to work.
Take action and evaluate the results
- Do not ignore any complaints and every complaint should be assessed. If the child has pain, discuss with the child/caregiver if any intervention is required. For e.g. do you want me to do something to help? Do you think we need to do something to relieve the pain? (Parents).
- Interventions do not necessarily mean analgesics as sometimes–simple measures like massaging or touching might be adequate for mild pain. On other occasions, just simple reassurance that the pain is accounted for and does not signify anything else serious might be adequate.
- After an intervention, always reassess the child to check the response.
When should pain be assessed?
It is recommended that pain should be assessed under the following situations:
- At regular intervals–as the 5th vital sign o done when undertaking other routine assessments (other vital signs like BP, heart rate, respiratory rate and temperature). This is to avoid unnecessary distress or disturbance to the child.
- At other times like the time of admission, discharge, transfer, whenever the child or caregiver report of pain, after administration of pain medication, during and after painful procedures including all surgeries.
Tools for assessing pain in children
There are various tools/pain rating scales for children. A tool, which is selected to assess pain in children, must be appropriate not only for the chronological age but for also developmental age.
- As pain is a subjective experience, individual self–report is often favored. Self–report tools are appropriate for most children aged 4 years and older and provide the most accurate measure of the child’s pain.
- It is important to be sure that children, especially those between the ages of 3 to 7 years are competent to provide all the information regarding pain.
- Children over the age of 7 or 8 years, who understand the concept of order and number, can use a numerical rating scale.
- When communication is difficult, behavioral observation can be utilized but health professionals must be careful when interpreting pain behavior. This is because pain expression can be affected by the physical state (e.g. cognitive impairment), emotional state (e.g. depressed), coping style as well as family and cultural expectations.
- Always ensure that enough time is provided for the children to complete their pain assessments accurately.
- The suggested tools to be used for the various age groups are as below:
- 1 month–3 years: FLACC–this is a observational behavioral assessment and can be done by observing the child for 2–5 minutes.
- 0 > 3–7 years: Wong–Baker FACES Pain Rating Scale–this is a self–report tool whereby a child is asked to choose a face which best describes his pain. This is a simple and quick measure but children can sometimes get confused with happiness measure.
- 0 > 7 years: numerical scale–this is a self–report tool whereby the child is asked to rate his pain based on a numerical scale whereby ‘0’ is no pain, ‘10’ is the worst pain experience. (Refer Appendix 1,2,3,4 for pain assessment tools
Management of Pain
*Relieving measure include touch, distraction, music, deep breathing, heat or cold packs besides the analgesics.
Guidelines in pediatric pain management
As healthcare professionals looking after children, one of our main responsibilities is to eliminate or minimize pain and suffering whenever possible. It has been well documented that in this regard, a substantial percentage of children have been under treated. One of the main reasons is that many have fears of adverse effects of analgesic medications which include respiratory depression and addiction whilst some just feel that addressing pain in children simply takes too much time and effort.
Key concepts in pain management
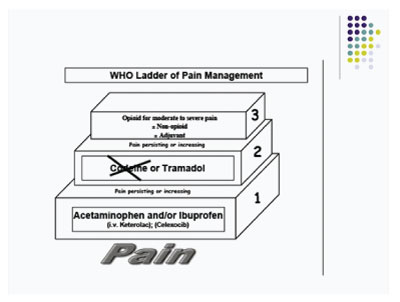
- “By the ladder” Enabling a stepwise approach to treatment commencing with non–opioids and increasing to strong opioids (Figure 1). The level at which a child enters the ladder is determined by the child’s needs, the intensity of pain and response to previous treatment
- “By the clock” Regular scheduling ensures a steady blood concentration, reducing the peaks and troughs of pro re nata (prn) dosing
- “By the appropriate route” Use the least invasive route of administration. The oral route is convenient, non–invasive and cost effective.
- “By the child” Individualize treatment according to the child’s pain and response to treatment.
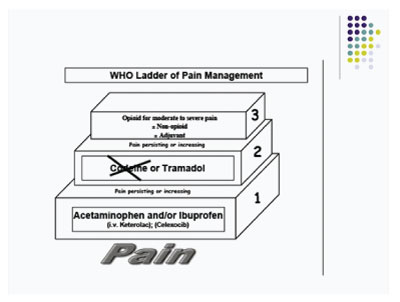
Figure 1: WHO Analgesic Ladder.
Step 1: Non-opioid + adjuvants
Step 2: Weak opioid + non-opioid + adjuvants
Step 3: Strong opioid + non-opioid + adjuvants
Methods of Pain Relief
Medications
- The non–opioid drugs like paracetamol and ibuprofen (and other NSAIDs) are more suitable for pain in musculoskeletal conditions, whereas the opioid analgesics are more suitable for moderate to severe pain, particularly of visceral origin.
- Paracetamol is the most commonly used analgesic with an excellent safety profile and lack of significant side effects. It is the mainstay for mild to moderate pain and is often combined with an opioid analgesic for more severe pain. Absorption of rectal paracetamol is slow, somewhat variable and comparatively inefficient.
- NSAIDs like Ibuprofen are indicated for mild to moderate pain. Children appear to have a lower incidence of renal and gastrointestinal side effects when compared to adults even with chronic administration.
- For a vast majority of children, opioids provide excellent analgesia with a wide margin of safety. With few exceptions, opioids should be administered to children via the oral or iv route. Intramuscular injections should be avoided unless necessary as children will deny they are in pain to avoid a shot.
Non Pharmacological interventions
a. Environmental factors
0 Create a child friendly environment which ensures privacy and comfort. Avoid bright lights or loud noisy places.
b. Other methods
Distractive techniques 0 Use age appropriate distraction strategies. This teaches the child to focus on something other than his pain. Children who worry too much about their pain will Non–opioid analgesics Paracetamol Non–steroidal anti–inflammatory drugs Ibuprofen Naproxen Diclofenac Meloxicam Opioid analgesics Weak opioid Tramadol Strong opioid Pethidine Morphine will Non–opioid analgesics Paracetamol Non–steroidal anti–inflammatory drugs Ibuprofen Naproxen Diclofenac Meloxicam Opioid analgesics Weak opioid Tramadol Strong opioid Pethidine Morphine
Often feel more pain than what is really there. Examples of distraction techniques include
- Holding a familiar object (comforter), such as pillow or soft cuddly toy.
- Singing; concentrating on nice things; telling jokes; games and puzzles.
- Blowing out air or bubbles.
- Reading pop–up books.
- Playing with a kaleidoscope or a 3D viewer.
- Breathing out (but not hyperventilating, which may increase anxiety and induce venoconstriction).
- Watching television or a video; playing interactive computer games.
- Listening to stories or music (through headphones)
Guided imagery: Teach the child to imagine that he is in his favorite place and doing his favorite things. By imagining he is in his favorite place will make him feel safe and relaxed and his pain may be decreased.
Information: Explain to the child what is going to happen during a procedure or surgery, this might decrease his nervousness and understand the pain that he might feel. This can decrease the fear of the unknown and pain can be decreased when the child believes that he can control and handle the pain
Music and Dance: Listening to music and dancing can ease the child’s pain and take the child’s mind off his pain or illness.
Heat and cold packs: Some types of pain are decreased by using heat whilst others might improve with cold
Massage and physical therapy: Massage, caress or stroking a child might make them more relaxed and soothe their pain.
Acknowledgements
This article discusses about the various pain management modalities in pain management, various pain scales, Infusion Pump, Syringes, Needles.
Conflict of Interest
Author declares there is no conflict of interest.
References
- Cancer pain relief and palliative care in children. WHO 1998
- Prevention and control of pain in children. Royal college of pediatrics and child health. 1997.
- Clinical practice guidelines. The recognition and assessment of acute pain in children. Available at: http://www.rcn.org.uk.
- Guidelines for Good Clinical Practice; Recognition and assessment of acute pain in children. RCPCH, UK.
- Medicines for children 2003, RCPCH 6. BNF for Children 2006
- American Medical Association, Module Pain Management: Pediatric Pain Management, September 2007.
- Tanne JH. Children are often under treated for pain. BMJ. 2003;327:1185.
- American Pain Society – APS: The assessment and management of acute pain in infants. http://www.ampainsoc.org.
- Non pharmacological Pain Management Therapies for Children. Available at: https://www.drugs.com/cg/non–pharmacological–pain–management–therapies–for–children.html.
- Birnie KA, Chambers CT, Fernandez CV, Forgeron PA, et al. Hospitalized children continue to report undertreated and preventable pain. Pain Res Manag. 2014;19(4):198–204.
- Birnie KA, Noel M, Chambers CT, Uman LS, et al. Psychological interventions for needle–related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2018;10(10):CD005179.
- Friedrichsdorf SJ, Postier A, Eull D, Weidner C, et al. Pain Outcomes in a US Children’s Hospital: A Prospective Cross–Sectional Survey. Hospital pediatrics. 2015;5(1):18–26.
- Shomaker K, Dutton S, Mark M. Pain Prevalence and Treatment Patterns in a US Children’s Hospital. Hospital pediatrics. 2015;5(7):363–370.
- Stevens BJ, Harrison D, Rashotte J, Yamada J, et al. Pain assessment and intensity in hospitalized children in Canada. The journal of pain: official journal of the American Pain Society. 2012;13(9):857–865.
- Taylor EM, Boyer K, Campbell FA. Pain in hospitalized children: a prospective cross–sectional survey of pain prevalence, intensity, assessment and management in a Canadian pediatric teaching hospital. Pain Res Manag. 2008;13(1):25–32.
- Twycross A, Collis S. How well is acute pain in children managed? A snapshot in one English hospital. Pain Manag Nurs. 2013;14(4):e204–215.
- Walther–Larsen S, Pedersen MT, Friis SM, Aagaard GB, et al. Pain prevalence in hospitalized children: a prospective cross–sectional survey in four Danish university hospitals. Acta Anaesthesiol Scand. 2016;61(3):328–337.