Purpose: Stereotactic brain biopsy is a frequently used method for diagnosing deeply located or diffuse intraparenchymal brain lesions and determining treatment options. Many comparative studies has been conducted between open surgical biopsy and framed and frameless stereotactic biopsy methods. In this study, we share the results, diagnostic sensitivity and experience of the cases who underwent stereotactic brain biopsy with frameless neuronavigation in our clinic.
Materials and Methods: The files of 41 patients who underwent stereotaxic biopsy with the help of frameless neuronavigation (MedtronicStealthStation S7) for deep-seated intraparenchymal, within important functional areas or adjacent, hard-to-reach lesions in our clinic between 2014 and 2021 were retrospectively reviewed. The patients’ age, gender, intracranial localization of the pathology, pathology results of the sample tissues and surgical operation results were evaluated.
Results: Of the 41 biopsied cases, 23 were male and 18 were female, and the mean age was 52.34 (16-78) years. While 3 (7.32%) of the patients who underwent biopsy for a parenchymal mass were lobar, 36 (87.8%) had a deep and prominent mass, and 2 (4.88%) had a diffuse mass that had migrated to the opposite cerebral hemisphere. High Grade Malignant Glial Lesion in 4 (9.76%) cases, Low Grade Glial Lesion in 7 (17.07%) cases, Metastasis in 2 (4.88%) cases, Glial Tumor in 1 (2.44%) case, 7 ( Anaplastic Astrocytoma (Who) Grade;3 ) 17.07%, Grade 2 Glial Tumor 1 (2.44%), Lymphoma 2 (4.88%), Glioblastoma (Who Grade) 9 (21.96%) cases IV, Diffuse Astrocytoma (WHO Grade II) ) ) 3 (7.32%) cases, Grade 2 Oligodendroglioma in 1 (2.44%) case, ischemia in 1 (2.44%) case and inflammation in 1 (2.44%) case. Non-tumor diagnosis was made in 2 (4.88%) cases diagnosed as Nonneoplastic Glial Tissues containing reactive changes.
Conclusion: In lesions located deep in the brain, difficult to reach, and in important functional areas, it is a great comfort for the patient to be able to diagnose with a stereotaxic method using a frameless method with neuronavigation without a large and huge craniotomy and without inserting nails into the scalp with a small burr hole.
Keywords: Biopsy, Intracranial Lesion, Frameless, Stereotaxy, Neuronavigation, Diagnosis
Despite the advances in neuroradiology and nuclear medicine, histopathological examination is required for the definitive diagnosis of most brain lesions and for the planning of treatments such as chemotherapy and radiotherapy [1]. Deeply located or without the possibility of resection; In addition to suspicious cases with diagnostic difficulties, stereotactic brain biopsy is used as a reliable diagnostic tool in cases where histological diagnosis is required for initiation of treatment [2]. Biopsy is also an option for patients who are elderly or have advanced disease who cannot tolerate craniotomy. Many studies evaluating the safety and efficacy of this procedure have been published, with an overall mortality rate of 0.7% and a morbidity rate of 3.5%. The diagnostic rate for this procedure is also around 90% [3]. In Despite the advances in neuroradiology and nuclear medicine, histopathological examination is required for the definitive diagnosis of most brain lesions and for the planning of treatments such as chemotherapy and radiotherapy [1]. Deeply located or without the possibility of resection; In addition to suspicious cases with diagnostic difficulties, stereotactic brain biopsy is used as a reliable diagnostic tool in cases where histological diagnosis is required for initiation of treatment [2]. Biopsy is also an option for patients who are elderly or have advanced disease who cannot tolerate craniotomy. Many studies evaluating the safety and efficacy of this procedure have been published, with an overall mortality rate of 0.7% and a morbidity rate of 3.5%. The diagnostic rate for this procedure is also around 90% [3]. In cases where removal of the mass is not considered, especially in the diagnosis of deeply located, diffuse infiltrative or multiple space-occupying lesions, biopsies performed with computerized tomography (CT) or MRI-guided stereotactic method have been proven to be safe and reliable in a wide variety of studies [4]. In the biopsy performed for the diagnosis of intraparenchymal tumors, many framed or unframed methods and mini-craniotomy and open surgery methods have been used. Neuronavigation devices are used in brain biopsy performed without a frame. The advantages and disadvantages of framed or unframed brain biopsy techniques are still the subject of ongoing debate; sampling accuracy, approach to deep brain lesions, and sample volume to name a few [5]. Apart from this, there are still debates about the deficiencies of craniotomy, open biopsy and stereotactic biopsy techniques in making a definitive diagnosis [6]. From this point of view, no definite superiority of any method over another has been demonstrated today. Here, it is obvious that the most important criteria determining the accuracy of diagnosis are patient selection and correct planning. For the first time in 1947, Spiegel and Wycisencephalotom developed the stereotaxic system that could be used in humans with the appliance they named [7]. Leksell, who is considered to be the pioneer of radiosurgery, described the stereotaxic coordinate determination method with the help of x-ray tomography [8]. Maroon et al. In the article they published in 1977, they reported three cases in which tumor biopsy was performed with the help of computed tomography (CT) and cyst or abscess aspiration was performed [9]. Biopsy from the brain by stereotaxic method is a safe, simple and high diagnostic value method. The technique can be applied with or without a fixed frame. Frameless computerbased navigation system is increasingly preferred. Patients have the advantages of tolerating the procedure more easily, taking less time, and being more economical. The percentage of reaching the correct diagnosis, complications and procedural mortality rates were not different from the procedures performed with the fixed frame system [10].
In this study, we shared the results, diagnostic accuracy and experience of the cases in which stereotaxic biopsy was performed with the help of neuronavigation for intraparenchymal lesions in our clinic.
Study Design
Forty-one patients who underwent biopsy with the help of frameless neuronavigation (Stealth Station S7®, Medtronic, Minnesota, USA) for cerebral intraparenchymal lesions in our clinic between 2016-2021 were retrospectively analyzed. Local ethics committee approval was obtained for the study. Of the 41 biopsied cases, 23 were male and 18 were female, and the mean age was 52.34 (16-78) years. While 3 (7.32%) of the patients who underwent biopsy for intraparenchymal mass were lobar, 36 (87.8%) had a deep and eloquent mass, 2 (4.88%) had a diffuse (diffuse) mass, which also passed to the opposite cerebral hemisphere (Table 1).
Preoperative Evaluation
All patients were evaluated preoperatively in terms of complete blood count, routine biochemical parameters and bleeding time. Preoperative administration of corticosteroids to patients was avoided unless there was very severe edema due to intracerebral lesions. Axial T2 CISS and axial T1 contrast magnetic resonance (MR) sections were taken from the patients at a 1 mm cross-section range suitable for the neuronavigation system and loaded into the neuronavigation device (Figure 1a,b,c).
Surgical Technique
In all cases, biopsy was performed without frame by the same surgeon (IA) using the Medtronic Stealth Station S7® (Stealth Station S7®, Medtronic, Minnesota, USA) brand and model neuronavigation system. Axial T2 CISS and axial T1 contrastenhanced magnetic resonance (MR) sections were taken from the patients with a 1 mm cross-section range suitable for the neuronavigation system and loaded into the neuronavigation device. All cases were fixed to a 3-pin Mayfield nail head with head position in accordance with the biopsy plan under general anesthesia. The cases were introduced to the patient navigation device using the neuronavigation system surface marking technique. Navigational drift was checked and patients with significant drift were reintroduced to navigation. Different points of the lesion were targeted in a way that would not affect or cross the shortest and most important areas and pathways most suitable for the lesion. The entry point was rechecked by navigation with an appropriate skin incision, and accordingly, using Stealth Station S7® (Stealth Station S7®, Medtronic, Minnesota, USA) neuronavigation surgical instruments with an average of 1.5 cm burr hole, 8 mm long and 1 mm thick. Biopsies were taken in all 4 directions and at different depths and sent to the histopathology department for frozen biopsy during the operation. Frozen pathology samples were taken in all cases with frozen biopsy results, and the surgery was terminated (Figure 2). Computed tomography was performed in all cases against the risk of early postoperative surgical complications (Figure 3) and all cases were monitored for 1 day and followed in the surgical intensive care unit.
Table 1:
Sex |
Age |
Localızatıon |
Hıstopathologıcal Dıagnosıs |
Hıstochemıstry |
M |
66 |
Right parietooccipital deep |
High Grade Malignant Glial Lesion |
GFAP: Positive |
F |
54 |
Near the corpus callosum and splenium |
High Grade Malignant Neoplasm |
GFAP: Positive |
M |
41 |
~24x17 mm in left thalamus |
Low Grade Glial Lesion |
GFAP : Positive |
F |
41 |
Deeply located in the right frontal 19*13mm |
Metastasis |
GFAP: Negative |
M |
64 |
Bilateral parietal right 22 mm left 9 mm |
Non-Neoplastic Glial Tissues Containing Reactive Changes |
GFAP: Positive |
F |
67 |
A 38 x 51 x 58 mm mass infiltrating both lateral ventricular corpus-posterior horns, extending to both centrumsemiovale, bitemporoparietal region |
Compatible with Glial Tumor |
GFAP : Positive |
M |
69 |
Left frontobasal |
Grade 3 glial Tumor |
GFAP : Positive |
F |
35 |
Right frontabasal |
Grade 2 glial Tumor |
GFAP : Positive |
M |
43 |
Craniocaudal 20 mm mediolateral size 15 mm lesion involving the cingulate gyrus on the right and an area of 47 mm superiorly |
Low grade Glial Tumor |
GFAP : Negative |
M |
52 |
Lesion involving the left side of the left frontoparietal corpus callosum |
lymphoma |
GFAP: Negative |
M |
33 |
17x21 mm lesion adjacent to the right thalamus |
Low Grade Glial Tumor |
GFAP: Positive |
F |
78 |
In the right occipito-parietal region ~2 cm |
Carcinoma Metastasis |
Pansitokeratin: Positive |
M |
71 |
Axial plane involving both sides of the corpus callosum splenium |
Glioblastoma (Who Grade IV |
GFAP : Positive |
M |
36 |
On the right, ~3x2 cm extending from the level of the centrum semiovalede to the body of the caudate nucleus and the lateral ventricle |
Anaplastic Astrocytoma (Who Grade;3) |
GFAP : Positive |
F |
16 |
Approximately 30x21mm in the axial plane medial to the right thalamus, approximately 8x6mm in the right lateral ventricle temporal horn medial |
Diffuse astrocytoma (WHO Grade II |
GFAP: Positive |
M |
54 |
left temporal deep |
Anaplastic Astrocytoma (Who Grade;3) |
GFAP : Positive |
F |
48 |
Left Parietooccipital deep |
Glioblastoma (Who Grade IV |
GFAP: Positive |
M |
65 |
right temporal deep |
Grade 2 oligodendroglioma |
GFAP: Positive |
F |
63 |
left thalamus |
Low Grade Glial Lesion |
GFAP : Negative |
M |
54 |
The right lateral ventricle is adjacent to the occipital horn. |
Diffuse astrocytoma (WHO Grade II |
GFAP: Positive |
F |
|
Medial to the right thalamus, approximately 17 mm in the axial plane, medial to the temporal horn of the right lateral ventricle. |
Diffuse astrocytoma (WHO Grade II |
GFAP: Positive |
M |
43 |
Right frontabasal |
Glioblastoma (Who Grade Iv |
GFAP : Positive |
M |
48 |
Lesion involving the left side of the left frontoparietal corpus callosum |
Glioblastoma (Who Grade Iv |
GFAP: Positive |
F |
44 |
The right lateral ventricle is adjacent to the occipital horn. |
Anaplastic Astrocytoma (Who Grade;3) |
GFAP : Positive |
M |
70 |
In the right occipito-parietal region |
Glioblastoma (Who Grade Iv |
GFAP: Positive |
F |
65 |
Right parietooccipital deep |
High Grade Malign Glial Lesion |
GFAP: Positive |
F |
55 |
lesion extending to the caudate nucleus body neither to the lateral ventricle |
Anaplastic Astrocytoma (Who Grade;3) |
GFAP : Positive |
M |
45 |
Lesion involving the left side of the right frontoparietal corpus callosum |
Glioblastoma (Who Grade Iv |
GFAP: Positive |
F |
43 |
right frontalbasal |
Low Grade Glial Lesion |
GFAP : Negative |
F |
66 |
Lesion adjacent to the lateral ventricle in the right frontoparietal region |
Non-Neoplastic Glial Tissues Containing Reactive Changes |
GFAP: Positive |
M |
36 |
Deeply located in the right frontal region, close to the base |
Low Grade Glial Lesion |
GFAP : Negative |
M |
48 |
Left insular region deep |
Anaplastic Astrocytoma (Who Grade;3) |
GFAP : Positive |
F |
56 |
Left pariataoccipital deep |
Glioblastoma (Who Grade Iv |
GFAP: Positive |
M |
71 |
Medial to the left thalamus, medial to the temporal horn of the lateral ventricle approximately |
Glioblastoma (Who Grade Iv |
GFAP: Positive |
M |
43 |
right frontalbasal |
Low Grade Glial Lesion |
GFAP : Negative |
F |
47 |
left temporal deep |
B-cell Lymphoma |
GFAP : Negative |
F |
47 |
Left parietal deep region |
demyelinated areas |
GFAP : Negative |
M |
48 |
lesion extending to the caudate nucleus body neither to the lateral ventricle |
Anaplastic Astrocytoma (Who Grade;3) |
GFAP : Positive |
F |
55 |
Lesion involving the left side of the left frontoparietal corpus callosum |
Glioblastoma (Who Grade Iv |
GFAP: Positive |
M |
66 |
Left Parietooccipital deep |
High Grade Malign Glial Lesion |
GFAP: Positive |
F |
42 |
right frontalbasal |
inflammatory cells |
GFAP : Negative |
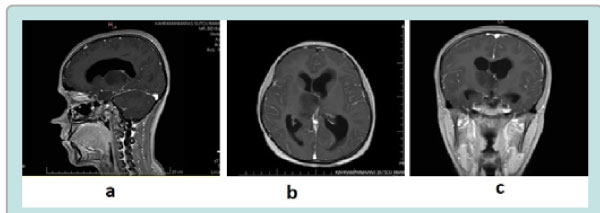
Figure 1: Figure-1a,b,c: Pre-operative axial, sagittal and coronal T1weighted Contrast magnetic resonance image.
Statistical analysis
The data were analyzed using Statistical Package for Social Sciences program version 20.0 for Windows (SPSS, Inc., Chicago, Illinois, USA) program. Descriptive data were expressed as mean, standard deviation or median, minimum, and maximum values for quantitative variables, while categorical variables were shown as numbers and percentages.
Of the 41 biopsied cases, 23 were male and 18 were female, and the mean age was 52.34 (16-78) years. While 3 (7.32%) of the patients who underwent biopsy for intraparenchymal mass were lobar, the masses of 36 (87.8%) patients were deep and located in the eloquent area, while the mass of 2 (4.88%) patients was diffuse (diffuse) and passed to the opposite cerebral hemisphere. High Grade Malignant Glial Lesion in 4 (9.76%) cases, Low Grade Glial Lesion in 7 (17.07%) cases, metastasis in 2 (4.88%) cases, Glial Tumor in 1 (2.44%) case, 7 ( Anaplastic Astrocytoma (Who Grade;3) in 17.07%, Grade 2 Glial Tumor in 1 (2.44%) case, Lymphoma in 2 (4.88%) cases, Glioblastoma (Who Grade) in 9 (21.96%) cases IV), Diffuse Astrocytoma (WHO Grade II) in 3 (7.32%) cases, Grade 2 Oligodendroglioma in 1 (2.44%) case, ischemia in 1 (2.44%) case, and inflammation in 1 (2.44%) case. Non-tumor diagnosis was also made in 2 (4.88%) cases diagnosed with Non-Neoplastic Glial Tissues containing reactive changes (table 1).
As a complication, hematoma developed in our patient with left temporal type localization and resorbed in the follow-up. None of our patients developed a new deficit compared to the preoperative period. Hematoma, which did not exceed 2-3 mm cm and did not increase, was observed in two patients.
The main purpose of all framed, frameless and craniotomy and open surgery methods used for biopsy for cerebral intraparenchymal lesions is to be easy and reliable and to make an accurate diagnosis. Many studies have been done in the literature comparing framed or unframed stereotactic biopsy and open biopsy based on diagnosis. In all these studies, it was shown that 51-79% success was achieved especially in glioma staging, and the reason for this was sampling error and tissue scarcity [1,11]. With the advancement of technology, especially frameless stereotactic biopsy devices are increasing and being widely used. Even in the era of advanced neuroradiological imaging, stereotactic brain biopsy remains a valuable and indispensable tool for neurosurgeons. This process can be done with the stereotactic frame as well as without the need for a stereotactic frame after the development of frameless neuronavigation systems. Image-guided navigation systems are gaining in popularity as they do not require the often painful practice of frame placement, and accuracy rates comparable to frame-based systems are reported [12]. Technically, in order to obtain a stereotaxic biopsy, the lesion must be visible on CT or MRI and the lesion must be non-vascular. The patient should not have local sepsis, signs of bleeding diathesis and serious obstruction for surgery. Complications of the procedure include subdural hematoma, intracerebral hematoma, intratumoral hemorrhage, CSF fistula, various motor deficits, porencephaly, secondary wound infections, tumor cultivation, and mortality. One of the main problems is that a specific diagnosis cannot be reached histopathologically in stereotaxic biopsies. Soo et al.[20] reported this rate as 8.1%. They suggested heterogeneity in gliomas and minor errors in target selection and identification as reasons for the negative results.
In framed systems, diagnostic rates ranging from 81% to 99% have been reported [12]. In the present study, histological diagnosis was achieved in 92% of the biopsy cases, and this rate is consistent with the general literature. There are some issues that should be kept in mind in order to increase the probability of being diagnosed with this procedure. The point to be targeted first should be the margin, not the center of the lesion. In this way, specimens taken from lesions with necrotic centers can provide sampling of living tissue representing the biological and histological features of the tumor. On the other hand, moving too far from the center of the lesion towards its periphery will bring the risk of sampling the gliotic border between the lesion and the brain tissue, so care should be taken when selecting the area to be sampled. Another point about the biopsy procedure is that if the lesion is enhancing, it should be targeted especially at the region with intense contrast enhancement [13,14,15,16,17,18,19]. Targeting high-grade localization, especially in heterogeneous glial tumors, is important for appropriate treatment planning. FLAIR, T2 weighted sequences, and MR spectroscopy fused with other images can be utilized when targeting non-contrast-enhancing lesions [21]. Biopsies taken from one direction at different depths or from different points using different directions also increase the probability of obtaining a diagnosis. In a study comparing biopsies taken from a single direction with different directions, it was shown that the procedure provides a higher rate of diagnosis when the first method is used [22]. Despite the disadvantage that the use of intraoperative MRI prolongs the procedure, Czyz et al. recommended intraoperative low-field MRI-guided procedures [23]. Lu et al. claimed that the percentage of reaching a positive diagnosis in brain biopsies performed under the guidance of magnetic resonance spectroscopy was higher than in MRI-guided procedures [24]. Dammers et al. examined their cases in which they performed stereotaxic biopsy in two separate time periods. Although they found the positive pathology diagnosis rate to be 89.4% between 1996 and 2000, they reported that this rate increased to 98.2% in the period of 2006-2010, which consisted of 160 cases. They suggested that the reasons for this development are standard surgical procedures and frozen-section when deemed necessary by the surgeon [25]. In our series, 2 patients out of 41 could not be diagnosed and the diagnostic rate was determined as 95.22%. When the undiagnosed patients were examined, it was seen that both patients had biopsies from a single point, not from different tumor points, which were performed in the early stages of the surgical procedure. Our high rate; It was thought that it was effective to always perform the surgical procedure by the same physician, to wait for the forzen results, and to take samples from different tumor localizations.
It is reported in the literature that perioperative complications range from 6% to 12%; however, mortality or permanent morbidity rates range from 0% to 2% and 3% to 6%, respectively [26]. The most common complication after stereotactic biopsy is bleeding at the operation site. Surgical infections and woundrelated complications are much less common than bleeding [26]. Bernstein reported the complication rate as 6.3% (19 patients) in biopsies taken from intraaxial lesions in his series of 300 cases, and five patients (1.7%) died in the series. The cause of mortality in these cases was subarachnoid hemorrhage and intracerebral hemorrhage in one patient each, and increased edema in three patients. The diagnosis was determined as glioblastoma multiforme in all patients with a mortal course. In the other 14 patients with complications, increased neurological deficits were detected due to bleeding. While these deficits were mild and transient in 10 patients, major deficits were observed in the other four patients [27]. Nishihara et al. investigated the rates and causes of morbidity in a stereotaxic biopsy series consisting of 56 cases. Neurological deficits developed due to intratumoral hemorrhage in three patients (5.2%). These bleedings were treated surgically. The pathological diagnosis was glioma in all three cases [28]. In the MEDLINE screening study covering the years 1998-2006, the morbidity rate was found to be 6.4% (37/575). The diagnosis of glioma was seen as a factor for morbidity, and it was emphasized to be very careful in terms of bleeding in biopsy from lesions located in the basal ganglia and thalamus. Malone et al. evaluated the complications seen after stereotaxic biopsy in their series of 7514 patients. While the most common complication was reported as bleeding (5.8%), infection was observed at a rate of 0.1% and wound dehiscence at a rate of 0.2%. It has been determined that hemorrhage is associated with age, hydrocephalus and edema, and it has also been reported that bleeding is less common after biopsy from primary malignant tumors. While mortality after biopsy was 2.8%, this rate was found to be 12.8% in patients with bleeding and 2.2% in patients without bleeding [26]. Shakal et al. In their stereotaxic biopsy series of 150 cases, they reported bleeding complications as 4.7% on post-biopsy CT [29]. Of these, 3.3% were symptomatic and 1.4% were asymptomatic. Metastatic tumors such as melanoma, choriocarcinoma, and renal cell carcinoma are more prone to bleeding. Stereotaxic biopsies are evaluated peroperatively mainly by cytological and "frozen-section" histological techniques. In our study, a 3 cm hematoma developed in the operation site in 1 patient with left insular temporal type, and no neurological deficit developed in the patient who resorbed in the followup. Approximately 2-3 mm of hematoma developed in 2 of our patients and there was no increase in bleeding in the follow-up. Our mortality rate was 0%. Frameless biopsy procedure has the same trajectory accuracy, rate of complications, and diagnostic yield like frame-based biopsy. But Not attaching the nails to the head with the frameless method reduces the possibility of nailrelated complications compared to the framed method and the possibility of headaches after surgery is reduced.
The relatively small number of cases and short follow-up periods are the limitations of our study.
Frameless stereotactic biopsy is superior to framed stereotactic biopsy methods in terms of patient comfort and operation time, and its mortality and morbidity is much lower than biopsy with open craniotomy [30]. With the contribution of navigation technology and the use of a frameless stereotaxic biopsy system, many benefits have been achieved in an MRI and CT compatible manner. In addition to having the same sensitivity as the conventional system, frameless stereotaxy has advantages such as better patient comfort, saving time and reducing costs. With this system, the discomfort caused by the fixation of the skull is prevented. In addition, the risks of complications such as fractures, CSF leakage and epidural hematoma that may develop due to the nailed head are eliminated [31].
It is a great comfort for the patient to be able to diagnose the lesions in deep-seated, hard-to-reach and important functional areas of the brain by neuronavigation and stereotaxic method with a frameless method without a large and large craniotomy, and without penetrating nails into the scalp with a small burr hole. We think that taking samples from different points of the lesion by paying attention to important and functional areas of the brain, pathways and vascular structures will increase the chance of success, and that this procedure will be performed by experienced hands and the rate of more accurate diagnosis will increase with an experienced neuropathologist.